 A toenail that has turned black, whether suddenly or gradually, can be an alarming sight. Sometimes, a toenail may turn black following repetitive injuries to the nail. In many cases, the nail can grow out naturally, but in more severe cases when the nail begins to lift off of the nail bed, medical attention will be required. A one-time blunt force injury, like dropping a heavy piece of furniture on your toes, can also turn your toenail black and often causes pain and swelling. Fungal nail infections typically cause toenails to turn white or yellow, but as debris builds up near the infection, the toenail can also turn black. Natural changes in pigmentation that can occur with age may turn the nails darker in people with darker skin. Other potential causes of black toenails include melanoma, and underlying medical conditions such as diabetes, kidney disease, heart disease, and anemia. If you notice a change in the color of your toenails, it is suggested that you seek the care of a podiatrist.
A toenail that has turned black, whether suddenly or gradually, can be an alarming sight. Sometimes, a toenail may turn black following repetitive injuries to the nail. In many cases, the nail can grow out naturally, but in more severe cases when the nail begins to lift off of the nail bed, medical attention will be required. A one-time blunt force injury, like dropping a heavy piece of furniture on your toes, can also turn your toenail black and often causes pain and swelling. Fungal nail infections typically cause toenails to turn white or yellow, but as debris builds up near the infection, the toenail can also turn black. Natural changes in pigmentation that can occur with age may turn the nails darker in people with darker skin. Other potential causes of black toenails include melanoma, and underlying medical conditions such as diabetes, kidney disease, heart disease, and anemia. If you notice a change in the color of your toenails, it is suggested that you seek the care of a podiatrist.
For more information about treatment, contact one of our podiatrists of Lovely Foot Associates, PC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our office located in Johnstown, PA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
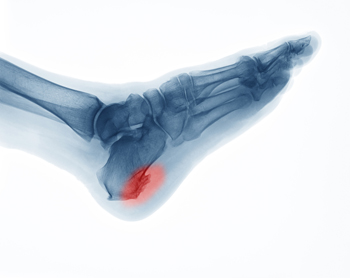 A common symptom of a heel spur is pain in the heel and surrounding areas. It is defined as a bony growth that forms on the bottom of the heel, and can cause severe pain and discomfort. It often occurs in patients who have plantar fasciitis, which affects the band of tissue that connects the heel to the toes. It can occur as a result of standing on hard surfaces, and walking for the majority of the day. It can be properly diagnosed by having an X-ray taken, which is necessary in determining how severe it is. Mild relief can be found when the affected foot is elevated, and the activity that caused the gradual development of the heel spur is temporarily ceased. If you are afflicted with heel pain, it is suggested that you schedule an appointment with a podiatrist as quickly as possible who can diagnose and treat heel spurs.
A common symptom of a heel spur is pain in the heel and surrounding areas. It is defined as a bony growth that forms on the bottom of the heel, and can cause severe pain and discomfort. It often occurs in patients who have plantar fasciitis, which affects the band of tissue that connects the heel to the toes. It can occur as a result of standing on hard surfaces, and walking for the majority of the day. It can be properly diagnosed by having an X-ray taken, which is necessary in determining how severe it is. Mild relief can be found when the affected foot is elevated, and the activity that caused the gradual development of the heel spur is temporarily ceased. If you are afflicted with heel pain, it is suggested that you schedule an appointment with a podiatrist as quickly as possible who can diagnose and treat heel spurs.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from Lovely Foot Associates, PC. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Johnstown, PA . We offer the latest in diagnostic and treatment technology to meet your needs.
The human foot has 26 different bones, and the foot is divided into three parts: the hindfoot, the midfoot, and the forefoot. Each section of the foot is composed of a different amount of bones. For instance, the forefoot is made up of 19 bones. The midfoot is composed of five smaller bones called the navicular, cuboid, and three cuneiform bones. Lastly, the hindfoot is made up of only the talus and the calcaneus. The feet tend to be vulnerable to slipping and twisting; consequently, fractured bones within the foot are common. When a bone gets crushed, bent, twisted, or stretched it may become broken.
Many foot fractures occur through an accident or trauma. More specifically, common causes for broken feet are car accidents, falls, missteps, or overuse. If you have a broken ankle or foot, you may have one or more of the following symptoms: throbbing pain, swelling, bruising, tenderness, deformities, and difficulty walking.
There are some factors that may put you at a higher risk of developing a broken foot. People who participate in high-impact sports are more likely to develop foot fractures because of the stresses, direct blows, and twisting injuries involved in gameplay. Additionally, those who suddenly increase their activity level are more likely to suffer a stress fracture.
Unfortunately, there are different complications that may arise because of a foot fracture. For instance, arthritis may be caused by fractures that extend into the joints. Bone infections are also possible in open fractures due to the bone being exposed to bacteria. However, there are ways you can help prevent yourself from breaking your foot. One way to avoid fractures is to wear proper footwear. If you plan on going on a run, you should wear running shoes. You should also replace your shoes if you notice that they are becoming worn out. For runners, it is best to replace shoes every 300 to 400 miles.
Treatment for foot fractures usually consists of rest, ice, elevation, and compression (RICE). If you plan on wrapping your foot, try not to wrap it too tightly because doing so may cut off blood supply in the foot. You should also avoid walking on the fractured foot.
If you suspect you have a broken foot, you should see your podiatrist right away. It is important that you have someone bring you to your doctor, since driving with a broken foot can be dangerous. You should especially seek urgent care if you are experiencing numbness, pain, or deformities in your foot.
 A broken foot can happen as a result of falling or enduring a sudden injury. The healing process can begin when a proper diagnosis is performed, which generally means having an X-ray taken. This is commonly followed by wearing a protective boot or cast, and it may help existing swelling when the foot is frequently elevated. The boot or cast may aid in walking while attempting to complete daily activities. If the fracture is severe, and the bone is protruding from the skin, surgery may be necessary for proper healing. It is suggested that you consult with a podiatrist if you have broken your foot.
A broken foot can happen as a result of falling or enduring a sudden injury. The healing process can begin when a proper diagnosis is performed, which generally means having an X-ray taken. This is commonly followed by wearing a protective boot or cast, and it may help existing swelling when the foot is frequently elevated. The boot or cast may aid in walking while attempting to complete daily activities. If the fracture is severe, and the bone is protruding from the skin, surgery may be necessary for proper healing. It is suggested that you consult with a podiatrist if you have broken your foot.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact one of our podiatrists from Lovely Foot Associates, PC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Johnstown, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
According to the American Diabetes Association (ADA), diabetes is a condition that affects approximately 23.6 million Americans. Around 750,000 new cases are diagnosed each year, and the disease’s most common form, Type 2 diabetes, makes up for 90 to 95 percent of these cases. Type 2 diabetes is especially prevalent among older Americans, those who are obese, and those who lead sedentary lifestyles.
Complications of the disease may lead to several foot and ankle-related conditions. The loss of nerve sensation, or neuropathy, can cause diabetics to lose feeling at the bottom of the feet and therefore leave them unaware of pain, pressure, and heat. Decreased circulation is another complication of diabetes that can slow down the healing of wounds and injuries; this can lead to the development of foot ulcers.
To prevent foot ulcers from forming, diabetics should examine their feet every day for small cuts and wear shoes that curtail pressure. Constant monitoring for the risk factors associated with ulcer formation can allow for early detection and therefore lessen the possibility of ulcers or, even worse, amputation. The removal of calluses and ingrown toenails should be left to the podiatrist to avoid improper removal and possible infection.
Diabetic patients may also experience foot deformities due to complications in their feet, such as limited joint mobility, muscle atrophy, and decreased fat padding. These complications can increase pressure in certain areas of the foot, which in turn can cause certain deformities, such as hammertoe, to form. Another deformity, Charcot foot, develops due to the collapsing of microfractures in the bones of the feet. The resulting deformity is a foot that is flattened and wider in appearance.
To help minimize pressure and prevent the development of these diabetes-related foot and ankle conditions, your podiatrist may consider using orthotics or special shoes. Charcot foot may be treated using walkers, custom orthotic insoles, or non-weight-bearing or rigid weight-bearing casts or braces. In more serious cases, surgery may be considered to treat more developed deformities. Ulcers can be further cared for with the help of proper diet, medication to control glucose, intensive wound care, and infection treatment.
 Dangers to the feet are a concern among diabetic patients. Complications could arise that affect the ability to feel cuts, bruises, and wounds on the feet, and can cause infections. A method that can keep the feet healthy can include monitoring glucose levels. Elevated sugar levels can be what causes a loss of feeling in the feet, and keeping a watchful eye may be helpful in preventing wounds and ulcers from developing. Many diabetic patients find it beneficial to place a mirror on the floor that can help to inspect the bottom of the feet. The feet need to be washed daily, and the toenails trimmed properly. There are many ways to protect the feet from diabetes. If you have this condition, it is suggested that you are under the care of a podiatrist who can help you to manage this ailment.
Dangers to the feet are a concern among diabetic patients. Complications could arise that affect the ability to feel cuts, bruises, and wounds on the feet, and can cause infections. A method that can keep the feet healthy can include monitoring glucose levels. Elevated sugar levels can be what causes a loss of feeling in the feet, and keeping a watchful eye may be helpful in preventing wounds and ulcers from developing. Many diabetic patients find it beneficial to place a mirror on the floor that can help to inspect the bottom of the feet. The feet need to be washed daily, and the toenails trimmed properly. There are many ways to protect the feet from diabetes. If you have this condition, it is suggested that you are under the care of a podiatrist who can help you to manage this ailment.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Lovely Foot Associates, PC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Johnstown, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.